# Coronary arterial anatomy
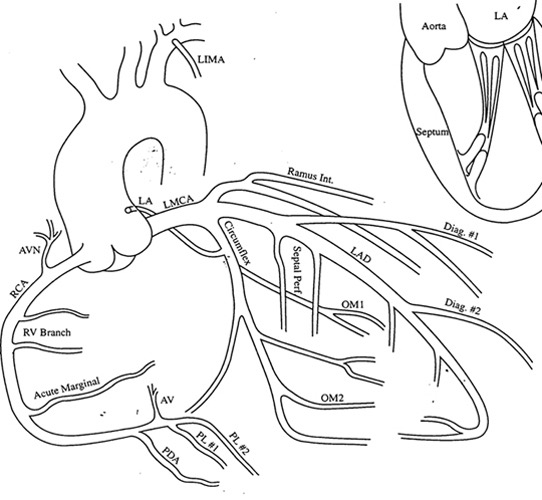
最重要的冠状动脉是左冠状动脉主干或左主干(LMS/LMCA),呈 C 形的供应下壁和右室血液的右冠状动脉。
左主干很快又分支成了两个血管:左前降支(LAD)和回旋支(LCA),LAD 供应了 60% 的心肌。
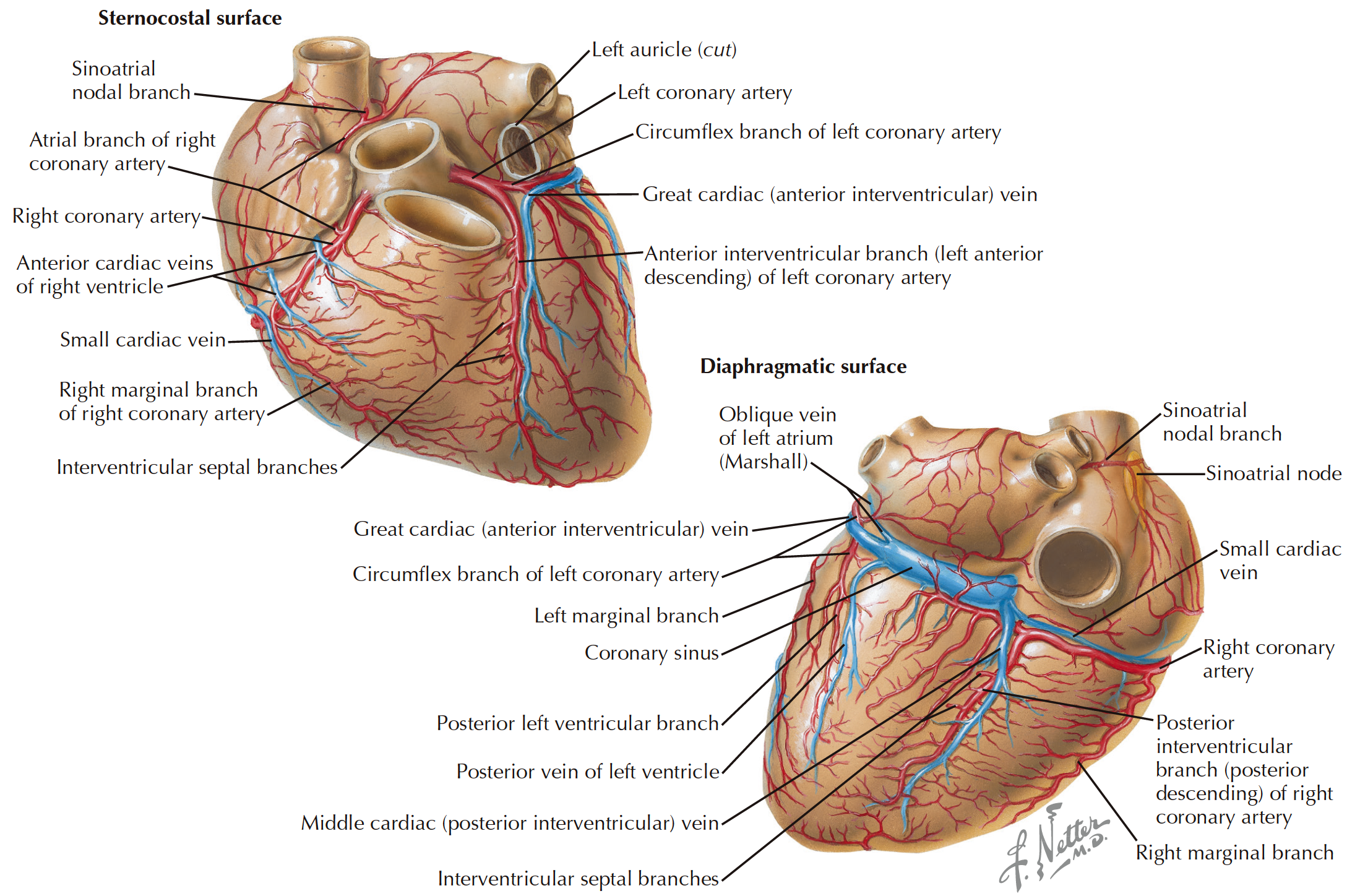
| Sternocostal surface | 胸肋面观 |
|---|---|
| Sinuatrial (SA ) nodal branch | 窦房结支 |
| Atrial branch | 房支 |
| RCA: Right coronary artery | 右冠状动脉 |
| Anterior cardiac veins | 心前静脉 |
| Small cardiac vein | 心小静脉 |
| Right marginal branch | 右缘支 |
| Interventricular septal branch | 室间隔支 |
| Left auricle | 左心耳 |
| LCA: Left coronary artery | 左冠状动脉 |
| CX: Circumflex branch | 旋支 |
| Great cardiac vein | 心大静脉 |
| Left marginal artery | 左缘支 |
| LAD: left anterior descending branch | 左前降支 |
| Diagonal branch | 斜角支 |
| Diaphragmatic surface | 横隔面观 |
|---|---|
| Oblique vein | 左房斜静脉 |
| Coronary sinus | 冠状窦 |
| Posterior left ventricular branch | 左室后支 |
| Middle cardiac vein | 心中静脉 |
| Posterior interventricular branch | 后室间支 |
# Right coronary artery
- Arises from the right sinus of Valsalva, ies between pulmonary conus and right atrium
发自右乏氏窦,位于动脉圆锥和右心房之间 - Moves sharply towards left of the observer and is directed towards sternum
快速向观察者左侧移动,并指向胸骨 - Curves down following right AV groove in direction of acute margin of heart and diaphragm
沿着右房室沟向心脏和横膈膜锐缘方向,向下弯曲 - Curves posteriorly and follows AV groove towards crux cordis.
沿着房室沟向心尖方向弯曲,向后弯曲
# Left coronary artery
投照角度:LAO 30-45°,CRAnial 25-35°
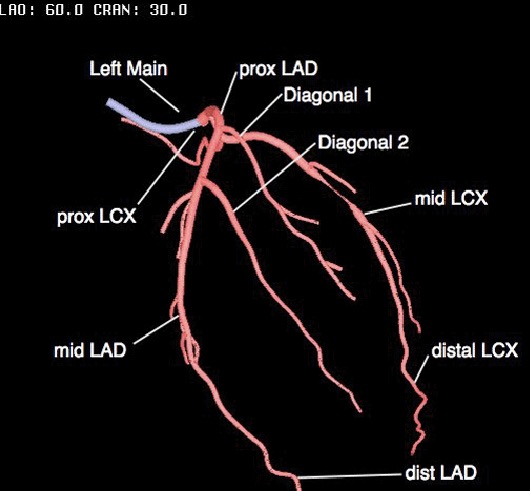
| Proximal | 近端 |
| Middle | 中段 |
| Distal | 远端 |
# Coronary Anatomy Correlates to LV Systolic Function 冠状动脉解剖与 LV 收缩功能相关
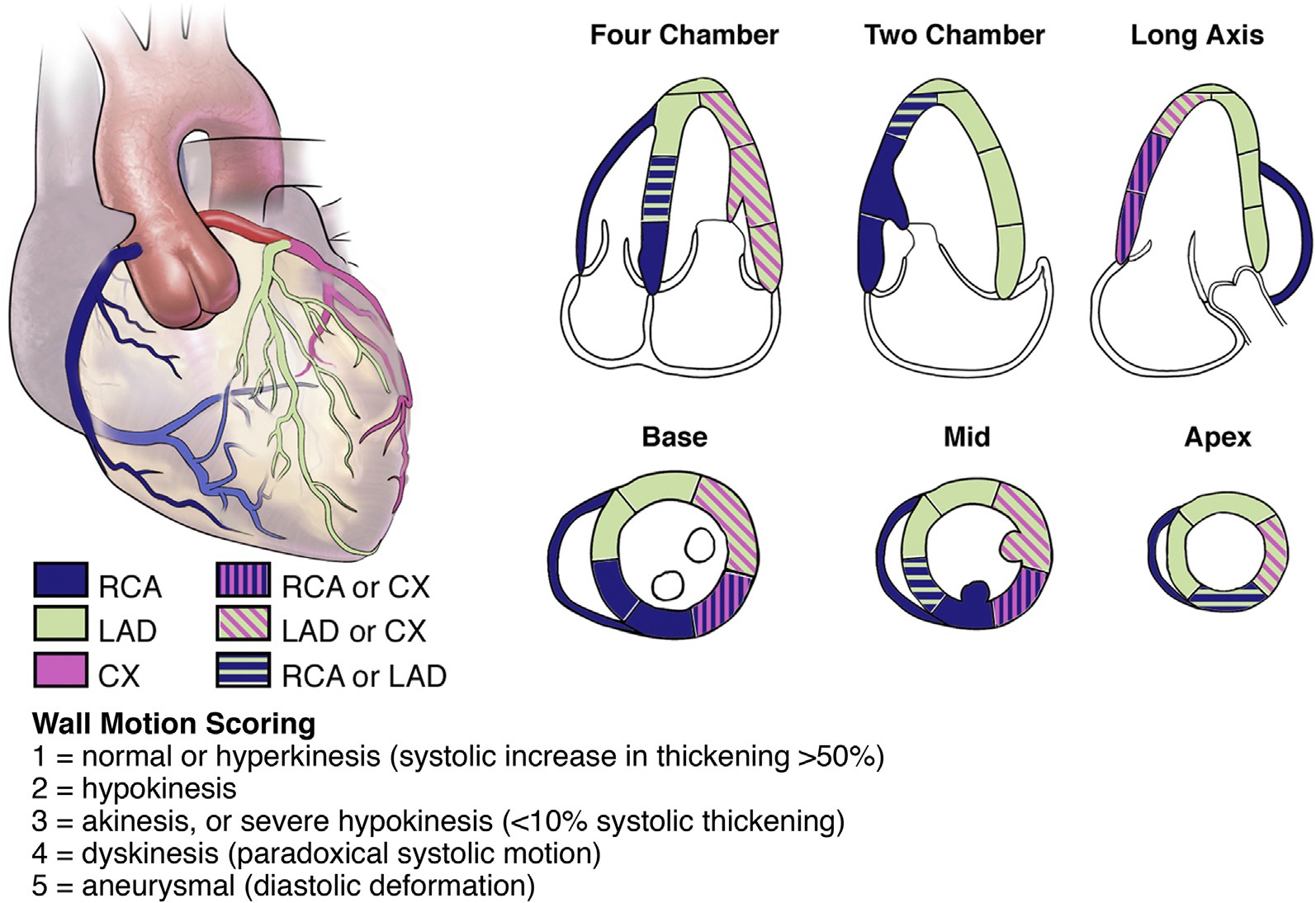
LAD - 左室前壁、室间隔的前三分之二、心室心尖部
CX - 左室前侧壁、下侧壁
RCA - 右室、室间隔的后三分之一、下壁
# LV 17 segment Model 节段模型
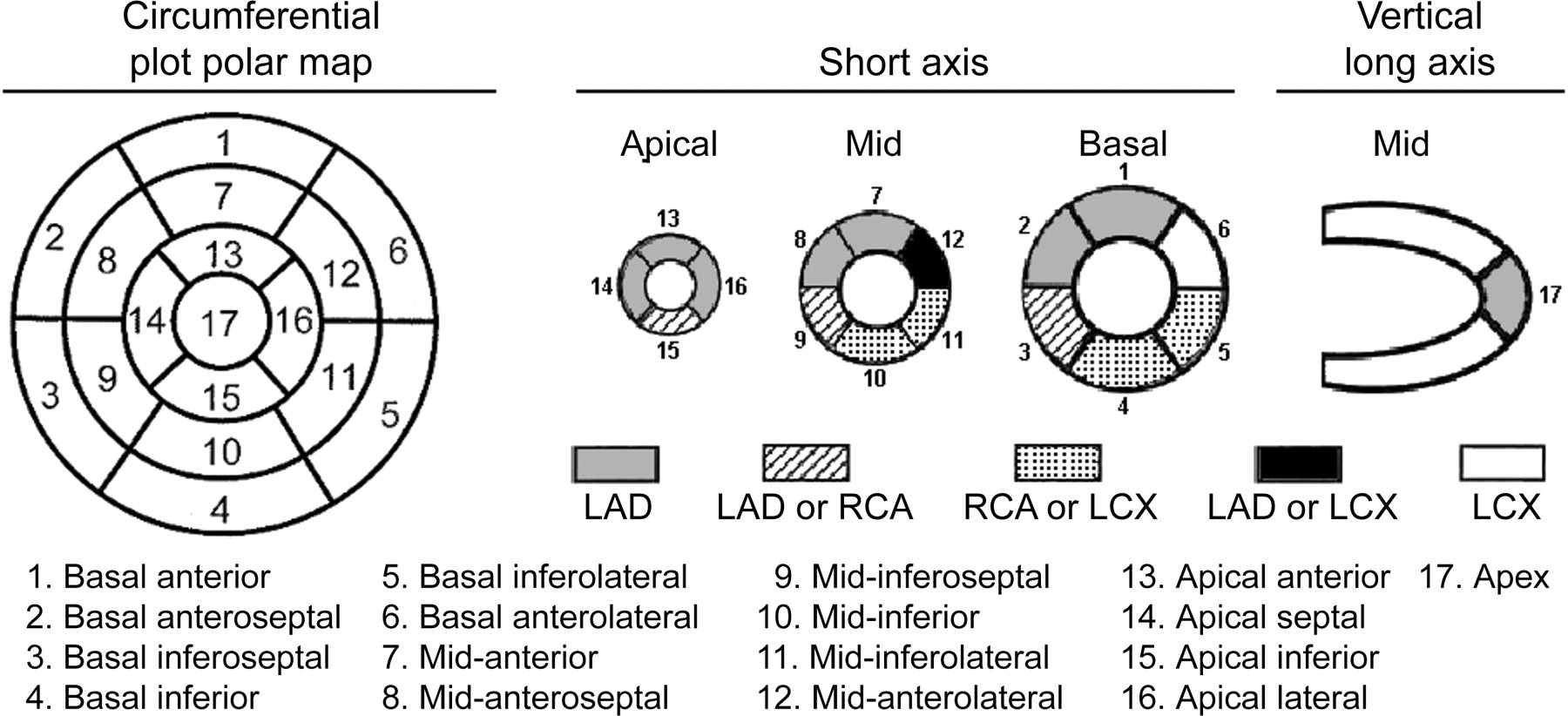
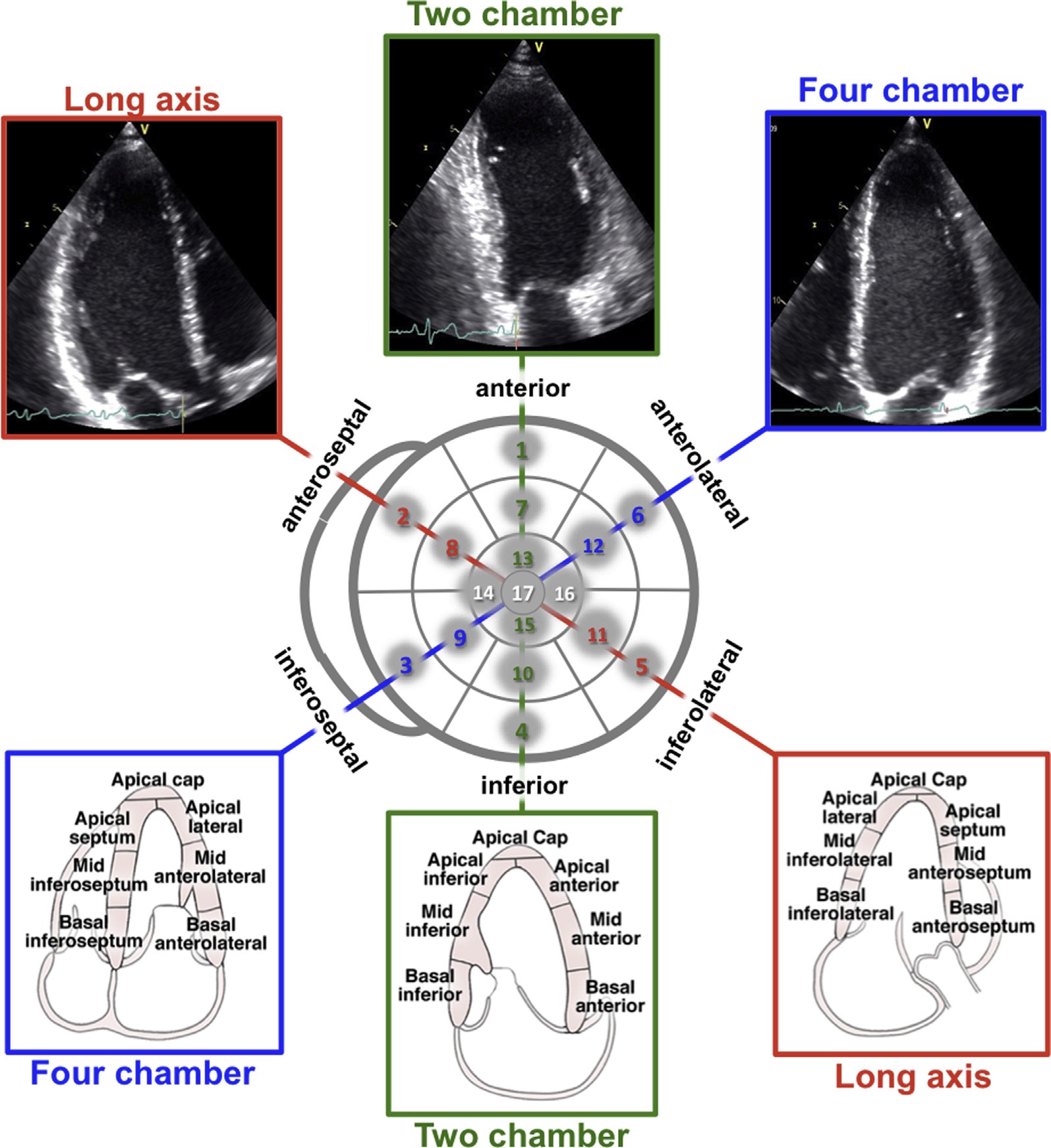
| Basal | 基底部 |
| Mid | 中部 |
| Apical | 心尖部 |
| Anterior | 前壁 |
| Anteroseptal | 前室间隔 |
| Inferoseptal | 后室间隔 |
| Inferior | 下壁 |
| Inferolateral/posterior | 下侧壁 / 后壁 |
| Anterolateral | 前侧壁 |
Note the anatomical correlates with the coronary arteries.
注意解剖结构与冠状动脉的关系。
The model is common for CMR, SPECT and PET allowing cross correlation.
这个编号模型和识别用法,被广泛用在了 CT、超声、MRI 中。超声有些困难,因为真实的心尖通常不容易看到。所以心超常参考 16 节段模型。
| CMR | cardiac magnetic resonance | 心脏磁共振 |
| SPECT | single-photon emission computed tomography | 单光子发射计算机断层成像术 |
| PET | positron emission tomography | 正电子发射断层成像术 |
# Segmental assessment
对每个节段进行功能描述
| Hypokinesia | 运动功能减退 | ≤ 40% wall thickening | 室壁增厚 < 40% |
| Akinesis | 室壁无运动 | <10% in systolic wall thickening | 室壁增厚 < 10% |
| Dyskinesis | 反向运动 | Wall moves OUTWARDS in systole | 室壁收缩期外向运动 |
WMS: wall motion score 室壁运动评分 or WMSI: wall motion score index 室壁运动评分指数:
- normal or hyperkinesis (systolic increase in thickening >50%)
正常或运动过度(收缩期增厚 > 50%) - hypokinesis
运动功能减退 - akinesis, or severe hypokinesis (≤10% systolic thickening)
运动不能,或严重运动减退(≤10% 收缩期增厚) - dyskinesis (paradoxical systolic motion)
反向收缩运动 - aneurysmal (diastolic deformation)
动脉瘤(舒张期变形)
- normal or hyperkinesis (systolic increase in thickening >50%)
WMSI = \frac{Total score of segments}
# Acute MI and its complications 并发症
AMI 患者在进入导管室行 PPCI(primary percutaneous coronary intervention /angioplasty 经皮冠状动脉介入治疗)之前,需要行超声心动图检查来评估左心功能
# Assessment
Assess overall LV function 评估整体左心功能,判断预后
- Simpsons Biplane method for LVEF 辛普森双平面法评估 EF 值
- LVEF < 40% suggests poorer prognosis
提示预后较差
- LVEF < 40% suggests poorer prognosis
- WMSI 室壁运动评分指数
- Score > 2 suggests poorer prognosis
提示预后较差
- Score > 2 suggests poorer prognosis
- Left atrial Volume Index 左房容积指数
- Values > 31 ml/m2 suggests poorer prognosis
提示预后较差
- Values > 31 ml/m2 suggests poorer prognosis
- Simpsons Biplane method for LVEF 辛普森双平面法评估 EF 值
Used routinely in our practice for patient assessment in the Heart Assessment Centre
常规用于心脏中心的患者评估- Assess acute regional wall motion abnormality to help diagnosis especially with non-specific ECG changes/ chest pain
评估急性节段性室壁运动异常以帮助诊断,特别是在有非特异性心电图改变 / 胸痛时 - Assess LV function and hence procedural risk
评估左室功能,从而评估手术风险 - Assess bystander valve disease
评估旁观者?瓣膜疾病 - Assess aortic root to reduce risk of missing aortic dissection; assess AR presence
评估主动脉根部以降低错过主动脉夹层的风险;评估 AR 的存在 - Assess presence of pericardial effusion.
评估是否存在心包积液
- Assess acute regional wall motion abnormality to help diagnosis especially with non-specific ECG changes/ chest pain
# MI Complications
# LV aneurysm 左室室壁瘤
- Deformity in BOTH systole and diastole (cf. segmental dyskinesia)
收缩期和舒张期畸形,向外出现膨出,收缩期较为明显(参见节段性反向的矛盾性运动) - Note risk of thrombus
注意血栓风险 - Note risk of arrhythmia.
注意心律失常的风险
# LV Pseudo-aneurysm 左室假性动脉瘤
- Essentially a rupture sealed by pericardium
实质上是室壁破裂,心室内的血液由破口进入心包腔,由心包黏连包裹形成 - Narrow perforation (neck diameter < 50% of the aneurysm diameter) with sharp edges;
超声下可以见到边缘锐利,彩色血流下可以看到较窄缩流颈的高速血流(缩流颈直径<动脉瘤直径的 50%) - Especially in the LCx (free wall) territory
经常出现在回旋支(游离壁)供血的区域 - Globular contour
呈现球形轮廓 - Wall expands with systole
收缩期室壁向外膨出 - PW Doppler at rupture shows 2 peaks (atrial and ventricular systole).
PW 放置在破裂口处时,可以看到 2 个波峰的频谱图(心房和心室收缩)
# LV thrombus 左室血栓
- Often associated with aneurysm
常与动脉瘤有关 - Common with full thickness MI
常见于透壁心梗 - Often apical (associated with LAD infarction)
通常出现在心尖部 (与左前降支梗塞相关) - Most seen within 2 weeks of the index event but 50% visualized within 48h
大多数在 2 周内出现,也有 50% 在 48h 内可见 - Echo findings: 心超表现
- Density HIGHER than adjacent myocardium
密度高于邻近心肌 - Contrast helpful for smaller thrombi
超声增强剂有助于较小血栓的检查,以区分肌小梁 - Adjacent to wall motion segmental abnormality
邻近室壁运动节段性异常 - Initially pedunculated then mural (and denser).
最初是有梗的血栓,随后会变成挂壁血栓 (更密集)。
- Density HIGHER than adjacent myocardium
# Mitral Regurgitation 二尖瓣反流
- Often no murmur
通常没有杂音 - Determine presence and severity of MR
超声需要确定 MR 的存在和严重程度 - Functional MR often related to postero-medial papillary muscle dysfunction and tethering
功能性 MR 通常与后内侧乳头肌功能障碍和栓系有关 - Annular dilatation with remodelling late post MI
心肌梗死后期,瓣环扩张重塑 - Associated with RCA/LCx infarction
与 RCA/LCx 梗塞相关 - In most severe and acute form: Papillary muscle rupture and acute severe MR
最严重和最紧急的情况:乳头肌断裂和急性重度 MR- This is with LOUD murmur and acute cardiogenic shock/haemodynamic compromise
伴有较大的响亮杂音和急性心源性休克 / 血流动力学不稳 - Often, florid pulmonary oedema.
通常有较重的肺水肿
- This is with LOUD murmur and acute cardiogenic shock/haemodynamic compromise
# VSD/Wall rupture 室间隔缺损 / 室壁破裂
VSD: ventricular septal defect 室间隔缺损
New loud murmur
新出现的响亮杂音Older age; female sex
高龄,女性Linked with history of hypertension
与高血压病史有关LV > RV; almost never in atria
发生于左室比右室多见,心房几乎从来没有出现过Occurs commonly in the anterior or lateral wall of the ventricle in the distribution areas of the left anterior descending coronary (LAD) artery
常见于左前降支(LAD)分布区的心室前壁或侧壁Occurs together with a relatively large trans-mural infarct involving at least 20% of the LV
发生于相对较大的透壁梗死,梗死范围至少累及 20% 的左心室Haemodynamic compromise
血流动力学不稳Milder in term of pulmonary oedema
肺水肿较轻Usually 2-7 days post MI
通常在 MI 后 2-7 天Much less common with PPCI and rapid reperfusion
PPCI 和快速再灌注后的发生率要低得多Occurs between 1 day and 3 weeks, but most commonly within 1-4 days in the wake of infarction.
发生在 1 天到 3 周之间,但最常见的是在梗死后的 1 到 4 天内。Happens at three distinct intervals and with three distinctive pathologic subsets.
室壁断裂根据发生的时间段不同,可以分为三个不同的病理亚型。
- Type I
- occurs early (within 24 hours) and is a full-thickness rupture, with its frequency rising owing to fibrinolytics.
I 型通常发生在早期(24 小时内),是透壁断裂,是因为纤维蛋白溶解导致其发生率升高。 - Type II
- happens 1-3 days post-MI and is in consequence of the erosion of the myocardium at the site of the infarction.
II 型发生在 AMI 后 1-3 天,是梗死部位的心肌受到侵蚀的结果。 - Type III
- occurs late and is situated at the border zone of the infarction and the normal myocardium.
III 型发生较晚,位于梗死心肌和正常心肌的交界区。
It has been hypothesised that type III ruptures may happen in the wake of increased wall stress secondary to dynamic LV outflow tract obstruction.
据推测,由于动态 LV 流出道阻塞继发的壁应力增加,可能会发生 III 型破裂。
Before PPCI VSD occurred in 3-5% of transmural or Q-wave MIs
在 PPCI 之前,3-5% 的透壁或 Q 波心梗会发生室间隔缺损Associated with high 30-day mortality rates
与 30 天的高死亡率有关VSD with an anterior infarct tends to be apical in location
前壁梗塞的室间隔缺损往往位于心尖部。RCA MI results in perforation of the basal inferior septum and has a worse prognosis than those in an anterior location (consider subcostal view)
RCA MI 导致下间隔基底部的穿孔,预后比前位穿孔更差 (考虑肋骨下切面)。The likelihood of survival depends on the degree of the impairment of the ventricular function and the size of the defect.
患者存活的可能性取决于心室功能受损的程度和缺损的大小。Diagnosis by echocardiography with Colour Flow Doppler Imaging. The actual defect may not be visible.
彩色多普勒超声心动图可以诊断。实际的缺陷可能看不到。Simple: Perforation is at the same level on both sides of the septum as a direct through-and-through communication.
简单:如果穿孔位于室间隔双侧的相同水平,可以作为直接的直通通信,彩色多普勒可以很好的看到分流情况Complex rupture is characterised by extensive haemorrhage with irregular, serpiginous tracts in the necrotic tissue in 30-40% of patients.
复杂破裂的特点:是 30-40% 的患者广泛出血,坏死组织形成不规则的曲线通道,不易被观察到。A large shunt is typified by the hyper-contractility of non-infracted LV segments with a low forward stroke volume, high pulmonary artery flow velocity, and elevated pulmonary artery systolic pressure.
大分流的典型特征是:无梗死的左室节段收缩亢进,伴有较低的前向搏出量,较高的肺动脉血流速度,和升高的肺动脉收缩压。
# RV infarction 右室梗死
Feature of RCA infarction 右室梗死的特点
- Presents with low cardiac output and low BP
表现为低心输出量和低血压 - No pulmonary oedema
无肺水肿
- Presents with low cardiac output and low BP
Echo features: 超声表现
- RV dilatatior
右室扩张 - Paradoxical septal motion
室间隔的矛盾性运动 - IVC dilatation
下腔静脉扩张 - Bulging of IAS to LEFT
房间隔凸向左房 - TR with Low PA pressures
三尖瓣反流伴有较低的肺动脉压 - PR with steep pressure half time (due to high right ventricular end diastolic pressure
RVEDP).
肺动脉瓣反流频谱图提示有较陡峭的压力减半时间 (由于高右室舒张末期压力)
- RV dilatatior
# Pericardial Effusion 心包积液
- Also small effusions common early post MI
心肌梗死后早期常见少量积液 - Higher incidence in trans-mural infarction, especially large anterior MI
透壁心肌梗死中发生率较高,尤其是前壁大面积心肌梗死 - May predict a poorer outcome/more complex course e.g.arrhythmia
可能预示较差的结局 / 更复杂的病程,例如心律失常 - May be reactive (Dressler's type); 7-10 days post MI
可能是心脏损伤后的综合征 (Dressler‘s 型);一般出现在心肌梗死后 7-10 天- Fever, polyserositis and severe pain.
表现为发烧、多发性浆膜炎和剧烈疼痛。
- Fever, polyserositis and severe pain.
# ECHO Assessment in Chronic CAD 评估慢性冠心病
- Markers of poor prognosis
预后不良的标志物- EF assessment
- Indication for ICD implantation (30%)
EF < 30% 则可能有 ICD 植入指征
- Indication for ICD implantation (30%)
- PW TDI septal annular velocity ≤ 3cm/s
组织多普勒测算瓣环速度 ≤ 3cm/s - LVEDD > 65mm
左室舒张末期最大直径 > 65mm - LA volume > 31ml/m2
左房容积 - Restrictive diastolic filling pattern (especially nonreversible)
限制性舒张功能障碍 (尤其是不可逆的) - RV fractional area change ≤ 32%; TAPSE < 14mm
右室面积变化分数 ≤ 32%;TAPSE < 14 mm - Pulmonary hypertension (TR peak velocity > 2.5m/s)
肺动脉高压 (三尖瓣反流峰值速度> 2.5m/s) - Secondary MR.
继发性二尖瓣反流
- EF assessment